Breathing and Blood Pressure, Pilot Test
Recently I’ve become fascinated with breath work though I’ve always been fond of mediation and other holistic practices — fancying myself…
Recently I’ve become fascinated with breath work though I’ve always been fond of mediation and other holistic practices — fancying myself a rather diverse health care provider. (Not to mention, as my newsletter and social handle imply — a cultured warrior / warrior poet!)
So, let’s get started with a quick mini-literature review (courtesy of @_branmckenzie and @shift_adapt).
There was a pretty comprehensive meta-analysis done in 2017 that reviewed cardiovascular measures (such as heart rate and blood pressure) and how they were effected by different breathing protocols.
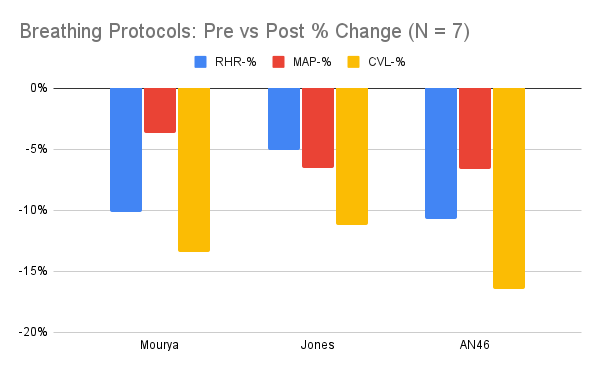
Two methods I found the referenced material (in the meta-analysis) for were Jones (2015) and Mourya (2009). So, these were the two protocols I used in my pilot testing.
Of note, these studies were typically any where from two weeks to three months in duration. What this means is that you may need to establish a longer term practice in order to see persistent results. For example, the Jones study was 2 months in duration and the Mourya study was 3 months in duration.
At any rate, their respective protocols (as I tested them) were as follows:
Jones:
15 min 1x / day (clinical trial was 30 min 2x / day)
Inhale:TotalResp ratio of 0.4; TotalResp = 10s
Mourya:
15 min 1x / day ( clinical trial was 15 min 2x / day)
Alt right and left nasal breathing 6in/6out
As you can see, I also added a third measure (AN46). This protocol was simply a combination of the two (Jones / Mourya) methods — a 04in:06out breathing cycle, alternating nostrils (one breath left, one breath right).
As I noted earlier, these results weren’t persistent day-to-day, meaning that my cardiovascular metrics returned to their “normal” levels by the time I began the breathing exercise the next day.
So, 1) I’m clearly looking into this more regarding long term (weeks / months) results; 2) having non-persistent results isn’t invaluable. A 10% reduction in your cardiovascular load is very significant even if temporary. As I work in mental health, this real-time biofeedback is very important for the implementation of coping strategies for say, anxiety / panic.
The phrases “deep breathing” and “breathing exercise” get thrown around as flippantly and cliche’ as “coping skills.” Without context, they are less than useless. Well, here is you’re context. If we establish a routine practice you can see your own biological metrics (you don’t even have to take my word for it — this is simple enough to do in-clinic) then you don’t have to “just believe” something will work in your time of crisis. You already have the data, you’ve already seen and felt the results with your own eyes and body.
This is a far more efficacious strategy than whimsically handing someone a “list of 100 coping skills” they’ve never practiced or used before and expecting them to be applied perfectly at a critically distressing moment. Similarly, telling someone to “take deep breaths” is about as helpful as telling them to “just calm down” during an argument — it’s not… ever.